

- OSTEOPOROSIS WITHOUT CURRENT PATHOLOGICAL FRACTURE TRIAL
- OSTEOPOROSIS WITHOUT CURRENT PATHOLOGICAL FRACTURE PLUS
OSTEOPOROSIS WITHOUT CURRENT PATHOLOGICAL FRACTURE PLUS
testosterone plus antiresorptive treatment in hypogonadal men). This is also important because, in secondary osteoporosis and osteoporosis associated with other comorbidities, rational and combined treatments could be offered (e.g. Thereby, further studies are needed to better understand the pathogenesis of male osteoporosis, define proper diagnostic criteria, and clarify the long-term anti-fracture potential of pharmacological agents. Indeed, vertebral fractures (VFs) were also reported in other trials (see subsequently), supporting the use of these drugs also in men. Although the main goal of treating men with osteoporosis is to decrease the risk of osteoporotic fractures, there is actually very limited evidence about the effects of therapies for osteoporosis in the male population.
OSTEOPOROSIS WITHOUT CURRENT PATHOLOGICAL FRACTURE TRIAL
Of note, very few studies assessed the effect of drugs for osteoporosis in men and only one large randomized controlled trial (RCT) provided data on fractures as primary endpoint ( 11). Furthermore, not only fewer men receive a correct and timely diagnosis of osteoporosis with respect to women, but also fewer men receive adequate treatment: antiresorptive therapy after a fracture has been reported for 4.5% of men with respect to 49.5% of women ( 9, 10). Indeed, evidence indicates that men tend to have more osteoporosis-related complications and the mortality rate associated with fractures is higher in men than in women ( 5, 6, 7, 8). As a consequence, identification of specific causes of male osteoporosis is essential to drive the correct treatment, and specific diagnostic procedures are needed in the management of osteoporosis in men. Actually, male osteoporosis is frequently secondary to other conditions and men tend to have more comorbidities ( 4). Guidelines on screening politics do not agree whether and when men should be considered, and clinical trials are far less performed in men with respect to women. The diagnosis, when even done, is often made late in the natural history of the pathology or even after a fracture event. While effectively less common in men than in women, osteoporosis affects both genders, but in men it is clearly under-estimated, under-diagnosed and under-treated. In contrast, very little has been done dealing with these aspects for osteoporosis in the male. In women, researches in the past decades clearly indicated the best strategies for prevention, screening, risk factor management, clinical management and treatment, and novel drugs have been developed to manage osteoporosis, fracture risk and complications, with many clinical trials performed ( 1, 2, 3). For too long time this pathology and its complications have been regarded as a typical female condition, whereas male osteoporosis has been neglected or under considered. Health disparities exist in the osteoporosis field. Introduction: gender differences in osteoporosis
This review focuses on the areas that are still nebulous in male osteoporosis field, from identification of subjects who need to be evaluated for osteoporosis and screening programs dealing with primary prevention to diagnostic procedures for good estimates of bone quantity and quality and precise calculation of fracture risk and personalized treatment that take into account the pathophysiology of osteoporosis. Of note, very few studies assessed the effect of antiosteoporotic treatments in men and most of them considered only bone density as primary endpoint. Furthermore, not only fewer men receive a correct and timely diagnosis, but also fewer men receive adequate treatment, and adherence to therapy is far less in men than in women. Moreover, men have more osteoporosis-related complications and higher mortality rate associated with fractures. Therefore, identification of specific causes of male osteoporosis is essential to drive a correct and personalized treatment.
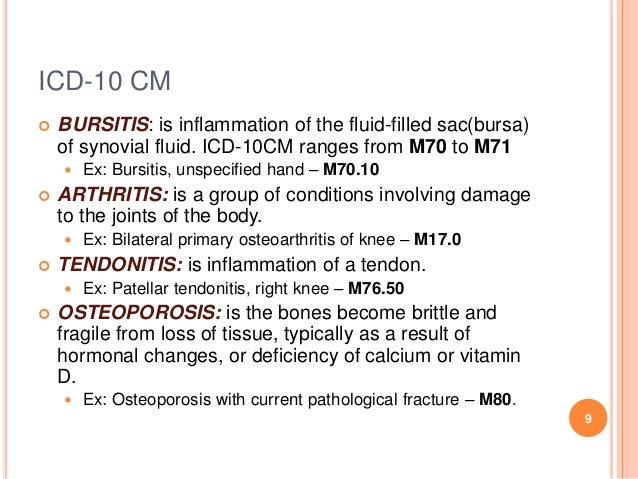
Male osteoporosis is frequently secondary to other conditions and often associated with comorbidities. Actually, most of our knowledge on male osteoporosis, especially regarding treatment, is extrapolate from the female counterpart. The diagnosis is often made late in the natural history of the pathology or even after a fracture event. This condition is clearly under-estimated, under-diagnosed and under-treated. Male osteoporosis has been neglected for too long time and there is need for a change.


 0 kommentar(er)
0 kommentar(er)
